Vaccine responses against SARS-CoV-2 variants examined in people with lupus 08 octobre 2021
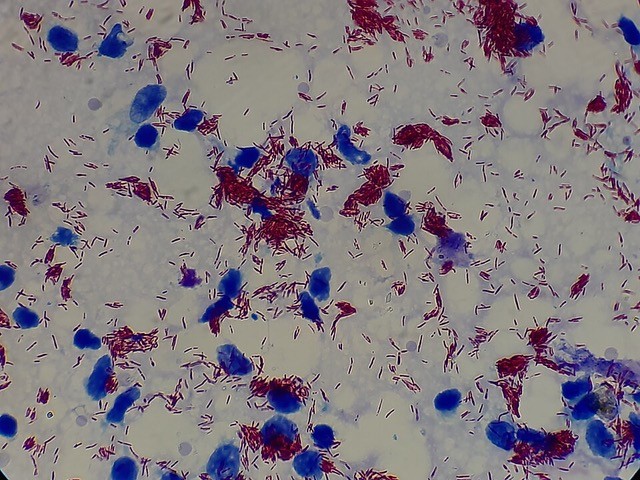
The majority of people with systemic lupus erythematosus (SLE) who respond to messenger (m)RNA COVID-19 vaccines also generate an antibody response against emerging SARS-CoV-2 variants, albeit with reduced neutralizing activity against variants bearing the E484K mutation, researchers report.
Zahir Amoura, from Sorbonne University in Paris, France, and study co-authors evaluated data from a total of 126 people with SLE (median age 47 years, 91% women) who received both doses of the Pfizer–BioNTech (BNT162b2) vaccine, with a 3–4-week gap between doses. A total of 23% had active SLE at baseline according to a SLEDAI 2K score of more than 4 points, while 17% had active disease according to a BILAG B score of at least 1 point.
In the subpopulation of 46 patients with serum samples measured against four major SARS-CoV-2 lineages, more than 80% produced neutralizing immunoglobulin (Ig)G antibodies against the D614G strain (the dominant circulating strain early in the pandemic) at the 42-day follow-up. All of these 37 patients also had neutralizing antibodies against the B1.1.7 (alpha) variant.
However, among these 37 patients, “serum neutralization activity decreased with lineages bearing the E484K mutation” in the receptor binding domain of the SARS-CoV-2 spike protein, say Amoura et al. The proportion of participants with neutralizing activity decreased to between 87% and 92% for the B.1.617.2 (delta), B.1.617.1 (kappa), B.1.1.28 (P.1; gamma), and B.1.617.3 variants, and to 60% for B.1.351 (beta).
“Altogether, these results demonstrated that vaccinated-SLE harboured decreased neutralising activity against [variants of concern], as previously described in vaccinated healthy donors,” say the researchers, but they stress that neutralizing responses “remained detectable in a majority of patients.”
In addition to their research on variants, the team also investigated predictors of vaccine immunogenicity – measured by titers of anti-SARS-CoV-2 IgG antibodies – in the full study population. They found that higher levels of total serum IgG and naïve B cells at baseline were associated with better seropositivity rates at day 42, while treatment with methotrexate or mycophenolate mofetil was associated with a “drastically reduced” antibody response.
Conversely, neither baseline disease activity nor treatment with hydroxychloroquine, steroids at high or low doses (median high dose=19 mg/day prednisone), or belimumab was associated with antibody response.
These findings “support the recommendation not to defer mRNA vaccination in patients with active SLE,” write Amoura and team in the Annals of the Rheumatic Diseases.
They note that while “[t]here is still controversy regarding the effect of steroids on SARS-CoV-2 vaccine efficacy,” the study results “suggest that patients with SLE with a daily dose of prednisone close to 20 mg should properly respond to BNT162b2 vaccine.”